Frequently Asked Questions
Kidney disease refers to a variety of conditions related to compromised kidney function. This includes acute kidney injury and chronic kidney disease. Many conditions can be considered the underlying cause loss of kidney function, like high blood pressure, diabetes, lupus disease, IgA nephropathy, and many others.
Acute kidney injury refers to any sudden loss of kidney function.
Some patients do not develop apparent symptoms. Acute kidney injury is noticed on routine labs for other purposes. When symptoms develop, they may include feeling weak, confusion, vomiting, urinating less, blood in the urine, swelling, or shortness of breath.
Inform your provider with any of the previous symptoms.
This depends on the underlying cause of the acute kidney injury. Your provider or nephrologist will investigate the cause of kidney injury and attempt to reverse the cause accordingly.
It is a progressive slow loss of kidney function. CKD typically occurs due to chronic injury of time by chronic disease processes like diabetes and hypertension. If untreated, it may lead to continued loss of kidney function and even dialysis.
Early on, chronic kidney disease causes no symptoms. As the disease advance, patient can develop feet/ankle swelling, uncontrolled high blood pressure, feel tired, or damage bone health.
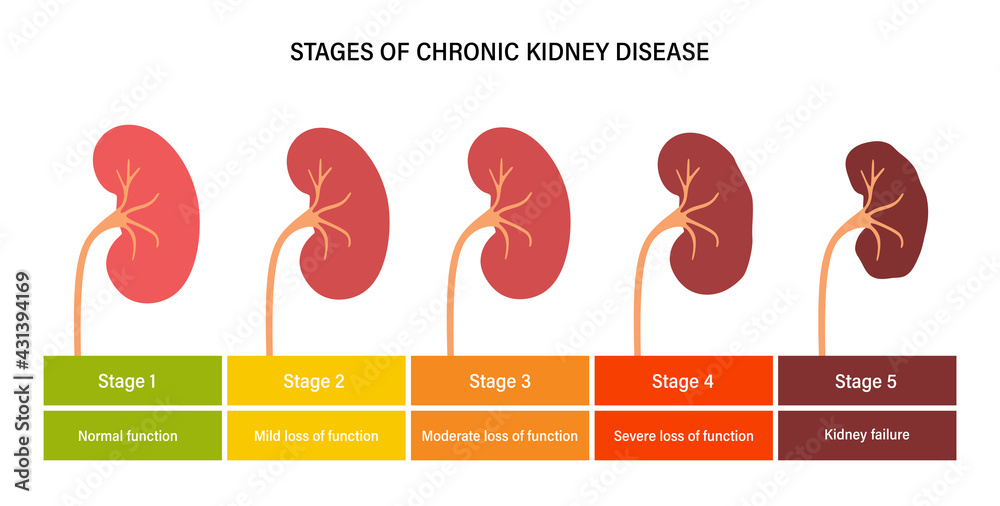
Chronic kidney disease is divided to five stages based on the glomerular filtration rate. Stages 1-3 are considered early stages, while stages 4-5 are advanced stages.
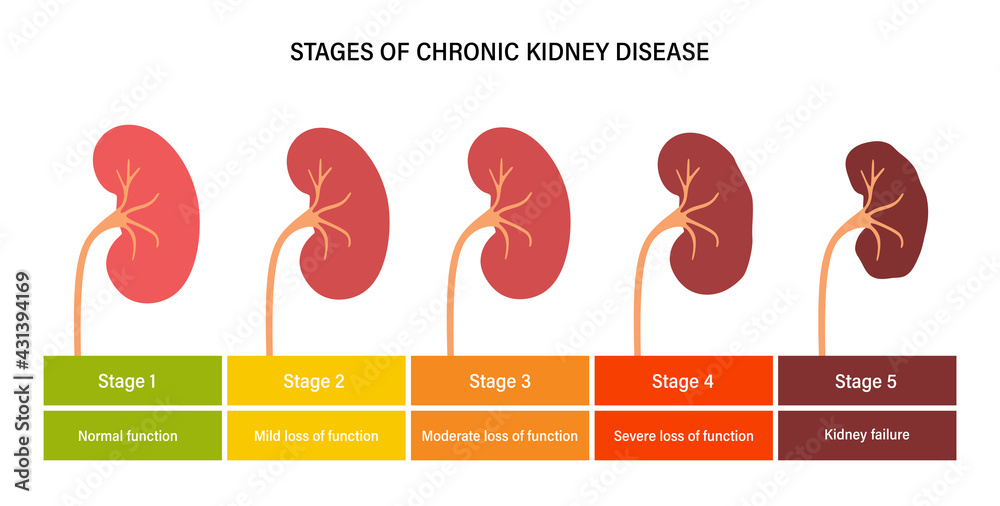
Dialysis is usually initiated at stage 5. Once in the advanced stages, preparation for dialysis or transplant start. Your nephrologist will start discussing treatment options and establish appropriate timeline.
Yes, kidneys can be protected to halt function loss. Visiting with a nephrologist and maintain regular follow ups helps achieve this goal. Controlling the underlying cause is important in this process.
Currently, the field of nephrology is seeing great achievement in the field of chronic disease. Patient with early stages of chronic kidney disease can be started on medications to help protect the kidneys.
Complete loss of function from progression of chronic kidney disease is considered permanent. There are two options to be offered in such case, initiating dialysis (home versus in-center) or kidney transplant.
This is a shared decision between the patient and his/her nephrologist. Determining the best treatment option would be based on multiple factors. Exploring these factors with your nephrologist is an important part of ensuring good outcomes.
There are two main types of outpatient dialysis; hemodialysis and peritoneal dialysis.
Hemodialysis is when a machine takes over the job of the kidneys. Blood is pumped from the body, filtered through a dialysis machine, and then returned to the body. There is In-Center Hemodialysis and Home Hemodialysis.
In-Center is done at a specialized center usually 3 times a week. Each treatment usually takes 3 to 5 hours. Home dialysis is done 3 to 7 times a week, but patients control their schedule. Each treatment usually takes 3 to 10 hours.
Peritoneal dialysis uses a special fluid that is placed into the belly. This fluid collects waste and excess salt and water from the blood. After that, the waste fluid drains out of the belly.
Kidney disease refers to a variety of conditions related to compromised kidney function. This includes acute kidney injury and chronic kidney disease. Many conditions can be considered the underlying cause loss of kidney function, like high blood pressure, diabetes, lupus disease, IgA nephropathy, and many others.
Acute kidney injury refers to any sudden loss of kidney function.
Some patients do not develop apparent symptoms. Acute kidney injury is noticed on routine labs for other purposes. When symptoms develop, they may include feeling weak, confusion, vomiting, urinating less, blood in the urine, swelling, or shortness of breath.
It is a progressive slow loss of kidney function. CKD typically occurs due to chronic injury of time by chronic disease processes like diabetes and hypertension. If untreated, it may lead to continued loss of kidney function and even dialysis.
Chronic kidney disease is divided to five stages based on the glomerular filtration rate. Stages 1-3 are considered early stages, while stages 4-5 are advanced stages.
Resources